Childhood Leukemia: Hope Through Gene Therapy

One of the most common cancers in children is leukemia. Acute lymphoblastic leukemia (B-cell ALL) is the most common form of this cancer in childhood. It is rare in adults. But the latest treatments for blood cancer have not only slowed the progression of the disease, they have even reversed the process. Therefore , the new type of gene therapy represents a ray of hope for the children affected.
But to understand leukemia, you should first know which cells it affects and how this disease develops. Everything starts in the bone marrow. It is a whitish, spongy tissue. It’s inside the long bones. For example, the thigh bone, the hip or the sternum.
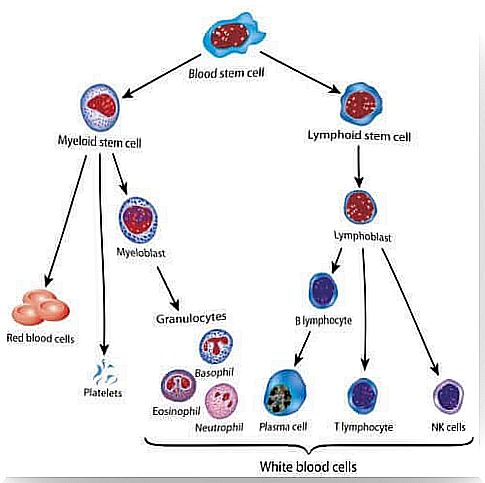
There are a small number of stem cells in the bone marrow. These are responsible for the formation of the various blood cells. They divide and develop into progenitor cells for the two lines of blood cells: lymphoid cells and myeloid cells (red blood cells, platelets, and some white blood cells). So how does B-cell leukemia begin?
Childhood Leukemia
Basically, every cancer develops in the same way: In the body, cells start to multiply in an uncontrolled manner for various reasons. The peculiarity here is that these degenerate cells do not die. Since your whole body is made up of cells, cancer can basically occur in any organ in the body.
In childhood leukemia, cancer originates in the bone marrow. Hence, the cells affected are the various blood cells. Especially those that make white blood cells or myeloid cells (myelocytes).
Sometimes these cancer cells stay in the bone marrow. But, as a rule, they end up in the bloodstream. And so they spread the disease. Also, in some cases, they can invade other parts of the body such as the lymph nodes, spleen, liver, and the central nervous system.
Types of childhood leukemia
Based on various characteristics, the American Cancer Society classifies childhood leukemia into the following subtypes: First, there is acute or fast-growing and chronic or slow-growing leukemia. In addition, depending on the cell type involved, a distinction is made between myeloid or lymphatic leukemia. Here is a brief overview:
- Acute lymphocytic leukemia (ALL). This is the most common type. It affects lymphocytic cells. These are the ones that make white blood cells. It is also known as B-cell leukemia.
- Acute myeloid leukemia (AML). This form comes from the myeloid cells. It is one of the forms with the highest likelihood of relapse.
- Chronic lymphocytic leukemia (CLL). It is very rare in children. It works on the white blood cells in the bone marrow.
- Chronic myeloid leukemia (CML). This variant has its origin in hematopoietic cells, which make red blood cells and platelets and thus enter the bloodstream. This form is rare in children.
A ray of hope: gene therapy
Recently, the Clinic de Barcelona hospital in Spain treated several children with B-cell leukemia. These children had not previously responded to conventional treatment. A new type of gene therapy with the active ingredient Tisagenlecleucel has now been applied to them. However, this is still in the experimental phase in humans.
This treatment was approved by the US Food and Drug Administration (FDA) in 2012. The distribution runs through the pharmaceutical company Novartis. But what exactly is gene therapy?
Gene therapy
Gene therapy is a treatment that is precisely tailored to each patient. This involves introducing specific genes into certain patient cells. This is how you want to fight diseases. In this way one avoids the rejection of transplants. And the effectiveness of the treatment is increased. Because you develop specific points of attack on cancer.
Treatment of childhood leukemia with gene therapy
The process consists of several steps and takes about 22 days.
- First, blood cells are taken from the patient and the T lymphocytes are isolated. T lymphocytes (circulating white blood cells) are responsible for the cellular immune response.
- Then you manipulate them genetically in the laboratory. Add a DNA sequence. This is how you reproduce a protein called CAR (Chimeric Antigen Receptor).
- The CAR recognizes cancer-specific proteins on the surface of the cancer cells, the so-called CD19.
- Now these modified T lymphocytes of the patient are multiplied in the laboratory.
- Finally , the modified T cells are injected into the patient intravenously.
How do the T-CAR / CD19 cells work?
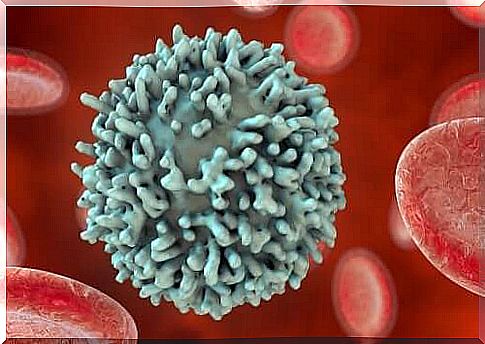
The best way to do this is to imagine the cells as a sphere with some branch-shaped structures emerging from the surface. Each of them has its very own morphology. These “branches” are responsible for the relationship of the respective cell to its environment as well as to other cells.
In this particular case, the patient’s modified T lymphocytes have a very specific “branch” on the surface. These are the CAR cells mentioned above. These are specifically designed to recognize another “branch” on the surface of the B cells, called CD19. After the T-lymphocytes have recognized the cancer-causing B-cells, they can now proceed to their elimination.
Still, there are things to consider. So says Dr. Francis Collins, Director of the National Institute of Health (NIH):
Successes and failures of immunotherapy in children with leukemia
According to the National Cancer Institute, which is part of the NIH , 80% of the patients who had not responded satisfactorily to conventional chemotherapy showed a marked remission of the disease.
However , in view of the observed side effects, this success of immunotherapy should still be viewed carefully. Dr. Collins submitted a report on the matter. The following points should be emphasized:
- The CD19 protein is found in B lymphocytes. Therefore, the LT-CDR does not differentiate between cancer cells and the healthy cells. And so the patient has to undergo immunosuppression.
- Occurrence of the cytokine release syndrome. However, this subsides after the use of suitable medication.
- There are also neurological side effects. This includes confusion and convulsions. However, these seem to decline again without the need for treatment.
Of course, this innovative treatment has given new hope to the families of the children affected. It has not yet been perfected and is in the experimental phase. But still have more permits than good results, the approval of immunotherapy to treat other cancers, such as HPV or lymphomas.